|
Fever
Your child has a fever if his
• Rectal temperature is over 38.0ºC
• Oral temperature is over 37.5ºC
• Axillary's (armpit) temperature is over 37ºC
The body’s average temperature when it is
measured orally is 37ºC. But it normally
fluctuates during the day. Mild elevation (38ºC
to 38.5ºC) can be caused by exercise,
excessive clothing, a hot bath or even on hot
days. Warm food or drink can also raise
the oral temperature. If you suspect such an
effect on the temperature of your child,
take his temperature again in one-half hour.
Causes
Fever is a symptom, not disease. Fever is the
body’s normal response to infections and
plays a role in fighting them. Fever turns on
the body’s immune system. The usual
fever (37.8ºC to 40ºC) that all children gets
are not harmful. Most are caused by viral
illnesses. Some are caused by bacterial
illnesses. Teething does not cause fever
usually..

Expected Course
Most fever of viral illnesses range between
(38.3ºC to 40ºC) and last for 3 to 4 days.
In general, the height of the fever does not
relate to the seriousness of the illness.
It is the behavior of your child which is more
important. How sick your child acts
is what counts. Fever causes no permanent harm
until it reaches 41.7ºC. Fortunately;
the brain’s thermostat keeps untreated fever
below this level.
Although all children get fevers, only 4%
develop a brief febrile convulsion. Since
this type of seizure is generally harmless, it
is not worth worrying about. Especially if
your child has had high fever before without
seizures.
Home Care
Acetaminophen products (panadol,
paracetamol) for reducing fever.
Children older than 2 months of age can be given
any one of the acetaminophen
products. Tylenol, panadol, and Tempra all have
the same dosage. Remember that
fever is helping your child fight the infection.
Use drugs only if the fever is over 38.5º
and preferably only if your child is also
uncomfortable. Give the correct dosage for
your child’s age every 4 to 6 hours, but not
more often. Two hours after they are
given, these drugs will reduce the fever 0.3ºC
to 1ºC. Medicines do not bring the
temperature down to normal unless the
temperature was not very elevated before the
medicine was given. Repeated dosages of the
drugs will be necessary because the
fever will go up and down until the illness runs
its course and the infection is taken
care off by the body. If your child is sleeping,
do not awaken him for medicines.
Caution: The dropper that comes with one product
should not be used with
other brands.
Dosages of Acetaminophen. As different brands
come in different strength, it is
important to give the correct dose as prescribed
4-6 hourly. Recommended dose
is 10mg/kg/dose either in tab or syrup form. Do
not over-load a child with
Paracetamol. Fever per se is harmless. However
liver damage caused by
excessive fever medicine can kill a child.
Liquid Ibuprofen. Ibuprofen and acetaminophen
are similar in their abilities to lower
fever, and their safety records are similar. One
advantage that ibuprofen has over
acetaminophen is its longer-lasting effect (6 to
8 hours instead of 4 to 6 hours).
However acetaminophen is still the drug of
choice for controlling fever in most
conditions. Children with special problems
requiring a longer period of fever control
may do better with ibuprofen.
Voltaren Suppository (Diclofenac Sodium)
May be given to a child if the temperature does
not settle 30 minutes after the oral
anti-fever medicines and the child is having a
lot of discomfort from the fever
( usually >39.5ºC). The suppository is best not
given to an infant less than 9 months
old. There is no necessity to sabotage the
body’s warfare against the germs by
aborting the fever if the child is comfortable.
Other Measures
Less clothing. Bundling can be dangerous;
clothing should be kept to the minimum
because most heat is lost through the skin. Do
not bundle up your child, it will cause
higher fever. During the time your child feels
cold or is shivering (the chills), give him
a light blanket.
Sponging This is usually
not necessary to reduce fever especially if your
child is
comfortable and you have just recorded a
temperature which scares you. Never
sponges your child without giving him
acetaminophen first. Sponge immediately
only in emergencies such as heat stroke
delirium, a seizure or any fever over 41
C. In other cases, sponge your child only if the
fever is over 40C, the temperature
stays that high when you take the temperature
again 30 minutes after your child
has taken acetaminophen and your chills is
uncomfortable. Until the fever
medicine has taken its effect (by resetting the
body thermostat), sponging will
just cause shivering which is the body’s attempt
to raise the temperate to that of
the raised thermostat temperature. Sponging
works faster then immersion so sit
your child in 2 ins (5 cm) of water and keep
wetting the skin surface. If your
child shivers, raise the water temperature a
little or wait for the fever medicine
to take effect. Don’t expect to get the
temperature below 38 C. Don’t add
rubbing alcohol to the water. It can cause come
if breathed in.
Extra fluids:
Encourage your child to drink extra fluids, but
do not force him to drink. Cooled
slightly chilled fluids are helpful. Body fluids
are lost during fever because of
perspiration.
Call at the A&E Department
Immediately if
• You are worry about your child condition and
your child is less than 2 months
old
• The fever is over 40.6C
• Your chills is crying inconsolably
• The child is poorly responsive
• Breathing is difficult and no better after you
clear the nose
• Your child has poor feeding for the whole day
and vomiting
• Your child acts and look very sick
Visit the clinic the next day
• Fever persists for > 72 hours
• Your child has had fever > 24 hours without
any obvious cause or location of
infection.
• Fever returns after it has gone away for more
than 24 hours
• Your child has a history of febrile seizure
Back to top
Vomiting
Definition
Vomiting is the forceful ejection of large
portion of the stomach contents through the
mouth.
The mechanism is a strong stomach contraction
against a closed stomach outlet. By contrast
regurgitation is the spitting of one or
sometimes more mouthful of stomach content,
which is
usually seen in baby less than 1 year old.
Cause
Most vomiting is caused by viral infection of
the stomach or eating something, which
disagrees with your child. Often the viral type
is associated with diarrhea. However vomiting
per se as a symptom could be a warning sign of a
more sinister condition. If vomiting is
persistent or in doubt, always consult a doctor.
Expected Course
The vomiting usually stops after 6-24 hours.
Dietary changes usually speeds up recovery.
Home care for vomiting
Special diet for vomiting
No solid for 8 hours
Start with clear fluids for 8 hours. Offer child
clear fluids (not milk) in small amount until 8
hours have
passed without vomiting. For vomiting without
diarrhea, the best clear fluid at any age is
water. For
infant, you can use any one of the new
electrolyte solution (pedialyte or hydralyte) or
rice water with
glucose can also produce excellent result. After
this age, soft drinks (100 plus, H two O) are
also
acceptable. Stir until no fizz remains (the
bubble inflate the stomach and increase the
chances of
continued vomiting).

Graduated feeding
Start with 1 teaspoon to 1 tablespoon, depending
on the age every 10 minutes. Double the
amount each hour.. If your child vomits using
this treatment, rest the stomach completely for
1
hour and then start over but with smaller
amounts. The one-swallow at a time never fails.
Bland food after 8 hours without vomiting. After
another 8 hours without vomiting, your child
can usually return to a normal diet.
For older children, starts with
food such as Marie crackers, honey or white
bread,
bland soups (eg chicken with stars), rice and
mashed potatoes.
For babies, start with food such as applesauce,
strained bananas and rice cereal. If your baby
only takes formula, give 1-2 ounces less per
feeding as usual. Usually your child can be back
on a normal diet 24 hours after recovery from
vomiting.
Diet for breast-fed babies. The key to treatment
is to provide breast milk at smaller amount
than usual. If your baby has only vomited once
or twice, continue breast-feeding but nurse on
only one side each time for 10 minutes. After 8
hours have passed since your baby last
vomited, return to both sides. If vomiting
occurs recurrently 3 or more times, put your on
water
or any rehydration solution. As soon as 4 hours
elapse without vomiting, return to nursing, but
again with smaller than the usual amount for 8
hours.
Medicine: Discontinue all medicine for 8 hours.
Oral medicine can irritate the stomach and
make vomiting worse. If your child has fever
over 39C and is uncomfortable use a Voltaren
suppository.
Common mistakes when treating
vomiting
A common error is to give the child as much
fluid as the child wants instead of gradually
increasing the amount. This almost always leads
to progressive vomiting. Keep in mind that
there is no effective drug or suppository for
vomiting and that dietary modification is the
answer. Vomiting alone per se rarely cause
dehydration unless drugs, which usually induce
vomiting, is continued, or too much milk or
fluid is given at one go.
Call at the A& E Dept
immediately if
Your child develops diarrhea and vomit more than
3 times greenish yellowish liquid (bilious)
No urine for > 12 hours
Crying produce no tears
Blood in vomitus not due to nose bleeding
Abdominal pain which last > 4 hours especially
if it is associated with reduced walking
Your child acts sick and become confused
Back to top
Emergency Symptoms
Some emergency symptoms are either difficult to
recognize or considered serious by
some parents when it is not. Most parents will
not overlook or underestimate the
importance of a major burn, major bleeding,
choking a convulsion, or a coma.
However, if your child has
any of the following symptoms, please contact
the A&E
Department immediately.
Sick
Newborn. If your baby is less than 1
month old and sick in any way, the
problem could be serious.
Lethargy, Fatigue
during an illness may be normal, but watch to
see if your child
stares into space, won’t smile, won’t play, is
too weak to cry, is floppy, or is hard
to awake. These are serious symptoms.
Severe Pain. If
your child cries when you touch or move him or
her, this can be a
symptom of meningitis. A child with meningitis
also doesn’t want to be held.
Constant screaming or
inability to sleep also point to severe
pain.
Can’t walk. If your
child has learned to walk and then loss the
ability to stand or
walk, he or she probably has a serious abdominal
problem such as appendicitis
or has injured a limb bad enough including a
fracture.
Tender abdomen.
 Press
on your child’s belly with your child sitting on
your leg Press
on your child’s belly with your child sitting on
your leg
and looking at his response. Normally you should
be able to press an inch or with
your fingers in all parts of the belly without
tenseness. It is significant if your
child pushes your hand away or screams. If the
belly is also bloated, the
condition is even more dangerous.
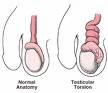 Tender
Testicle or scrotum This requires surgery
within 5 hours to save the Tender
Testicle or scrotum This requires surgery
within 5 hours to save the
testis.
Labored
Breathing. You should assess your child’s
breathing after you have
cleaned out the nose and when he or she is not
coughing. If your child has
difficulty in breathing, tight croupy breaths,
or obvious wheezing, he or she
needs to be seen immediately. Other signs of
importance include a bluish lips, or
retractions in between the ribs.
Bluish lips. Bluish
lips or cyanosis can indicate a reduced amount
of oxygen in
the bloodstream.
Drooling. The
sudden onset of drooling or spitting, especially
associated with
difficulty in swallowing, can mean that your
child has a serious infection of the
tonsils, throat, or epiglottis (top part of the
windpipe).
Dehydration.
Dehydration means that your child’s body fluids
are low.
Dehydration usually follows severe vomiting or
diarrhea. Suspect dehydration is
present if your child has not urinated for more
than 8 hours, crying produces no
tears, the mouth is dry rather than moist, or
the soft spot in the skull is sunken.
Dehydration requires immediate fluid replacement
by mouth or intravenously.
Bulging Soft Spot.
If the anterior fontanelle is tense and bulging,
the brain is
under pressure. Since the fontanelle normally
bulges with crying, assess it when
your child is quiet and in an upright position.
Stiff Neck. To test
for a stiff neck, lay your child down, then lift
the head until
the chin touches the middle of the chest, if he
or she is resistant, place a toy or
other object of interest on the belly so he or
she will have to look down to see it.
A stiff neck can be an early sign of meningitis.
Injured Neck. Discuss any injury to the neck,
regardless of symptoms, with your
child’s physician because of the risk of damage
to the spinal cord.
Purple Spots. Purple or blood red spots on the skin can be a
sign of a serious
Purple or blood red spots on the skin can be a
sign of a serious
bloodstream infection, with the exception of
explained bruises, of course.
Fever Over 105ºF (40.6ºC).
All the preceding symptoms are stronger
indicators
of serious illness rather than the level of
fever itself. All of them can occur with
low fever as well as high ones.
Fever becomes strong indication of serious
infection only when the temperature rises
above 105ºF (40.6ºC).
However an infant with any of the above symptom
without
fever could be very sick. If in doubt, always
seek medical opinion.
Back to top
Bronchiolitis
DEFINITION
Diagnostic Findings
• Wheezing: a high-pitched whistling sound
produced during breathing out
• Rapid breathing with a rate of over 40
breathes per minute
• Tight breathing (your child has to push the
air out)
• Coughing often with very sticky mucus
• Onset of lung symptoms often preceded by fever
and a runny nose
• An average age of 6 months, always less than 2
years
• Symptoms similar to asthma.
Cause
The wheezing is caused by a narrowing of the
smallest airways in the lung
(bronchioles). This narrowing results from
inflammation (swelling) caused by any of
number of virus, usually the respiratory sy
virus (RSV). RSV occurs in epidemics
almost every winter in the temperate country.
Whereas infants with RSV develop
bronchiolitis, children over 2 years of age and
adults just develop cold symptoms.
 This
virus is found in secretions of infected
individuals. This
virus is found in secretions of infected
individuals.
• It is spread by sneezing, coughing at a range
of less than 6 feet or by hand-to nose
or hand- to- eyes contact.
• People do not develop permanent immunity to
the virus.
Expected Course
Wheezing and tight breathing (difficulty
breathing out) become worse for 2 or 3 days
and then begin to improve. Overall, the wheezing
last approximately 7 days and the
cough about 14 days. The most common
complication of bronchiolitis is an ear
infection. Occurring in some 20% of infants.
Bacterial pneumonia is an uncommon
complication in only 1% or 2% of children with
Bronchiolitis. They are usually
hospitalized because they need oxygen or fluid
intake assistance. In the long run,
approximately 30% of the children who develop
bronchiolitis go on to develop
asthma. Recurrences of wheezing (asthma) occur
mainly in children who come from
families where close relatives have asthma.
Asthma is very treatable with current
medication.
HOME TREATMENT FOR
BRONCHIOLITIS
Medicines. Some children with
bronchiolitis respond to asthma medicines,
others less
so. However symptomatic medicines given by your
doctor will reduce your child’s
discomfort somewhat. Continue the medicine until
your child’s wheezing is gone for
24 hours. In addition, your child can be given
acetaminophen every 4 to 6 hours if the
fever over 102ºF (39ºC).
Humidity. Dry air tends to make cough
worse. Use a humidifier in your child’s
bedroom. The new ultrasonic humidifiers not only
have the advantage of quietness,
but also kill molds and most bacteria that might
be in the water.
Suction of a Blocked Nose. If the nose is
blocked up, your child will not be able to
drink from a bottle or nurse. Most stuffy noses
are blocked by dry or sticky mucus.
Suction alone cannot remove dry secretions. Warm
up water nose drops are better
than any medicine you buy for loosening up
mucus. Place three drops of warm water
in each nose. After about 1 minute, use a soft
rubber suction bulb to suck it out. You
can repeat this procedure several times until
your child’s breathing through the nose
becomes quiet and easy.
Feedings. Encourage your child to drink
adequate fluids. Eating is often tiring. So
offer your child formula or breast milk in
smaller amounts at more frequent intervals.
If your child vomits during a coughing spasm,
feed the child again.
No Smoking. Tobacco smoke aggravate coughing.
The incidence of wheezing
increases greatly in children who have an RSV
infection and are exposed to passive
smoking. Don’t let anyone smoke around your
child. In fact, try not to let anybody
smoke inside your home.
CALL AT THE A & E DEPARTMENT
IF
Your child stops breathing or passes out.
The lips become bluish
Your child starts acting very sick
Feeding is difficult for 12 hours especially if
associated with vomiting and
Breathing becomes labored or difficult.
The wheezing becomes severe (tight)
The chest retraction becomes severe
Breathing more than 60/mins
CALL AT THE OFFICE DURING
REGULAR HOUR IF
Your child is unable to sleep because of the
wheezing
Your child is not drinking enough fluids
A nasal discharge becomes yellow for more than
24 hours
Any fever (over100ºF [37.8ºC]) lasts more than
72 hours
Back to top
Hand Foot and Mouth Disease
Diagnostic Findings
• Small ulcers in the mouth
• A mildly painful mouth
• Small water blisters or spots located on the
palms and soles and
between the fingers arid toes
• Sometimes, small blisters or red spots on the
buttocks
• Fever (37.8ºc) may be as high as 40ºc
• Mainly occurs in children 6 months to 4 years
of age

Cause
Hand, Foot, and Mouth Disease is always caused
by a Coxsackie A virus. It has no
relationship to hoof and mouth disease of
cattle.
Expected Course
The fever and discomfort are usually gone by day
3 or 4. The mouth ulcers resolve in
7 days, but the rash on the hands and feet can
last 10 days. The only complication seen
with any frequency is dehydration from refusing
fluids.
Home Care
Diet. Avoid giving your child citrus,
salty, or spicy foods. Also avoid foods that
need
much chewing. Chang to a soft diet for a few
days and encourage plenty of clear
fluids. Cold drink, fruit juice are often well
received. Have your child rinse the mouth
with warm water after meals.
Fever. Acetaminophen may be given for a
few days if the fever is above 102ºF (39ºc).
Fever suppository if temperature is more than
39ºc and uncomfortable.
Contagiousness. Hand, Foot and Mouth disease is
quite contagious and usually some
of your child’s play mates will develop it at
about the same time. The is cubation
period after contact is 3 to 6 days. Because of
the rapid spread in childcare and playschool,
it is important to isolate your child to avoid
an epidemic. Please note that the
condition is seldom life threatening and no
undue anxiety is warranted.
Call at the
A&E Department if
• Your child has not urinated for more than 12
hours,
• The neck becomes stiff,
• Your child becomes confused or delirious,
• Your child becomes hard to awaken completely,
• Your child starts acting very sick.
During regular hours if
• Your child is not drinking much,
• The fever lasts more than 3 days,
• The mouth pain becomes severe,
• The gums become red, swollen, or tender,
• You feel your child is getting worse,
• You have other concerns or questions.
Back to top
Chickenpox
Diagnostic Findings of
Chickenpox
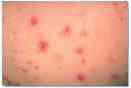
--Multiple small, red bumps that
progress to thin-walled water blisters; then
cloudy blisters or open
sores, which are usually less than 1//4 inch
across; and finally
dry, brown crusts (all within 24 hours)
--Repeated crops of these sores for' 4 to 5 days
--Rash on all body surfaces but usually starts
on head and back
--Some ulcers (sores) in the mouth, eyelids, and
genital area
--Fever (unless the rash is mild)
--Exposure to a child with chickenpox 14 to 16
days earlier
Chickenpox Virus
Cause
Chickenpox is caused by exposure to a highly
contagious virus 14 to 16 days earlier. A
chickenpox
vaccine is now available, given after the first
birthday.
Expected Course
New eruptions continue to crop up daily for 4 to
5 days. The fever is usually the highest on the
third or
fourth day. Children start to feel better and
stop having a fever once they stop getting new
"pox". The average child gets a total of 500
sores. Chickenpox rarely leaves any permanent
scars unless the soresbecome badly infected with
impetigo or your child repeatedly picks off the
scabs. However, normal chickenpox can leave
temporary marks on the skin that take 6 to 12
months to fade. One attack gives lifelong
immunity. Very rarely, a child may develop a
second mild attack.
HOME CARE
Itching and Cool Baths. The best treatment for
skin discomfort and itching is a cool bath every
3 to 4
hours for the first few days. Baths don't spread
the chickenpox for the first few days. If the
itching
becomes severe or interferes with sleep, give
your child a antihistamine
Fever. Acetaminophen may be given in the dose
appropriate for your child's age for a few days
if your
child develops a fever over 39° C. Aspirin
should be avoided in children and adolescents
with
chickenpox because of the link with Reye's
syndrome.
Sore Mouth. Since chickenpox sores also occur in
the mouth and throat, your child may be picky
about
eating. Encourage cold fluids. Offer a soft,
bland diet and avoid salty foods and citrus
fruits. If the
mouth ulcers become troublesome, have your child
gargle or swallow 1 table spoon of an antacid
solution four times daily after meals.
Sore Genital Area. Sores also normally occur in
the genital area. If urination becomes very
painful,
apply some lidocaine (Xylocaine) or 1%
Nupercainal ointment (no prescription needed) to
the genital
ulcers every 2 to 3 hours to relieve pain.
Prevention of Impetigo (Infected Sores). To
prevent the sores from becoming infected with
bacteria,
trim your child's fingernails short. Also, wash
the hands with an antibacterial soap (Cetaphil
or Isoderm)
frequently during the day. For young babies who
are scratching badly, you may want to cover
their
hands with cotton socks.
Contagiousness and Isolation.
Children with chickenpox are contagious until
all the sores have
crusted over, usually about 6 to 7 days after
the rash begins. To avoid exposing other
children, try not
to take your child school or childcare centre.
If you must see a doctor, leave your child in
the car with a
sitter while you check in to wait for your
child's turn. Most adults who think they didn't
have
chickenpox as a child had a mild case. Only 4%
of adults are not protected. If you lived in the
same
household with siblings who had chickenpox,
consider yourself protected. Siblings will come
down
with chickenpox in 14 to 16 days. The second
case in a family always has many more chickenpox
than
the first case.
Consultation
Immediately if your child develops
• a patch of red tender skin
• confusion and difficult to awaken
• trouble walking
• neck stiffness
• Breathlessness
• Vomiting
• bleeding into the chickenpox
• act sick with poor appetite Within 24 hours if
• the scab becomes larger
• The scabs become soft and drain pus. (NOTE:
Use an antibiotic ointment on these sores until
your child is seen by a physician.)
• The fever lasts over 4 days.
A lymph node becomes larger and more tender than
other
• The itching is severe and doesn't respond to
treatment
• Your child develops severe pain when
urinating.
• You have other concerns or questions.
Thing s happening before the typical pox appears
Febrile Fits
What Are Febrile
Fits?
Fits associated
with high fever are a common occurrence in
children. The incidence is about 4% in children
under five years of age.
The first fit usually occurs in a child between six months and
six years of age, who develops a high temperature of more than 38 degrees C. The high fever is usually caused by a viral infection
like a cold or a throat infection.
Simple febrile fits normally last less than 15 minutes and
involve clenching of teeth, up-rolling of the
eyes and jerking movements of all four limbs.
What Causes
Febrile Fits?
The cause of fits
with high fever is unknown. However, there is a
strong genetic predisposition, especially if
parents or siblings have a past history of fits.
What Are the
Chances of a Child Having Another Fit?
The recurrence
rate is higher in the younger child. If the
child is less than one year old, he has a 65
percent chance of having repeated fits. if the
child is between one to three years old during
the first fit then the recurrence rate is about
35 percent. The recurrence rate for a child
above three years old is about 20 percent.
Risk of Recurrent
Febrile Fits
Recurrence of
febrile fits is the largest risk for
children with this condition. The risk factors
for such recurrence are:
-
Early age of
onset (<
15 months)
-
Epilepsy in a
first degree relative
-
Febrile fits
in a first degree relative
-
Low degree of
fever (
<
40°C)
during first
febrile fit.
-
Brief duration
between onset of fever and initial fit
-
The chances
of recurrence is higher if the child has
been developmentally abnormal before the
first fit .

What Can Parents
Do to Minimise the Risk of Febrile Fits?
Measures must be
taken to prevent the fit by bringing down the
temperature. Anti-fever medications like "panadol"
must be given in the proper prescribed dose and
frequency. If a child still has a high
temperature, more than 39 degrees C despite
medication, then sponge the child with tepid
water or put him in the shower or bathtub. He
should wear light clothing.
Do not cover the
child with a thick blanket to "sweat it out".
What Does One Do
When A Child Throws A Fit?
Follow the
guidelines below and do not panic.
-
Put the
child's head down and to one side because
vomiting can occur after a fit. Allow the
child to throw out the vomitus, because if
the vomitus gets into the lungs then
aspiration pneumonia (chest infection) can
occur.
-
Do not try to
insert any objects (spoon, fingers) between
the child's teeth clenched during the fit;
he will not bite his tongue. By forcing his
mouth open, you may break his teeth and
cause bruising. This can be particularly
dangerous if the child swallows his broken
tooth into his windpipe during the fit.
-
Do not try to
arouse the child by pinching or bruising
him. These fits usually last a few minutes
and will stop spontaneously. No amount of
pain inflicted will wake the child up.
-
Bring the
child to the nearest doctor or hospital, and
if the fits do not stop then an injection or
insertion of medication rectally will stop
the fit. There is a risk of brain damage if
the fits are not stopped within half an
hour.
-
It is always
advisable to consult a doctor even after a
fit, to exclude more serious illnesses like
meningitis (infection of the brain). Your
child should be seen by a doctor if he
throws a complex fit, i.e. if the fit is not
associated with any fever, if he has more
than one fit in a day, if the fit is
prolonged (more than half an hour) or if the
jerking movements of the fits occur only in
some parts of the body.
Treatment
The treatment for
recurrent febrile fits is to prevent high fever
in your child. Sometimes your doctor may
prescribe medication if he thinks the fits will
recur again. Medications include:
-
Oral
anticonvulsants. These are anti-fit
medications which must be taken daily.
Treatment usually lasts for one or two
years.
-
Intermittent
use of rectal valium (a suppository) when
the child has a high fever.
Conclusion
Simple febrile
fits are common in children but it is usually
benign i.e. it produces no harmful effects.
Studies have shown that there is no
deterioration of academic performance in
children with simple febrile fits. Also not all
children who have high fever will have a fit.
Points to note:
Based on the above
discussion, the following approached is
recommended:
-
Parents of
children with
febrile fits should understand the
benign nature of this condition.
-
They should
know the effective measures of temperature
control such as tepid sponging with tap
water and antipyretic administration.
Paracetamol is still the safest antipyretic
and can be given at a dose of 15 mg/kg 6
hourly. Alternately NSAIDs can also be used.
The mechanism of action of tepid sponging
namely heat loss from the body surface
should be explained to the parents.
c. The parents
should also know the first aid measures during a
fit, if this was to recur:
i) Do not panic, remains calm. Note time of
onset of fit.
ii) Loosen the child's clothing especially
around the neck
iii) Place the
child in the left lateral position with the head
lower than the body.
iv) Wipe any
vomitus or secretion from the mouth
v) Do not insert
any object into the mouth even if the teeth are
clenched
vi) Do not give
any fluids or drugs orally
vii) Stay near the
child until the fit is over and comfort the
child as he/she is recovering.
viii) The
caregiver of children with a high risk of
recurrence, ie more than 3 risk factors, should
have a sup ply with a preparation of diazepam
rectal solution and should know how to
administer this in case the fit last more than 5
minutes.
ix) In the event
that the fit is not aborted by rectal diazepan,
parent should seek urgent medical help to stop
the fit before status epileptics develops.
x) If the fit is
aborted, parent should also seek medical advise
to determine the cause of the fever.
These
recommendations apply both to children who have
had a simple or a complex
febrile fit.
|